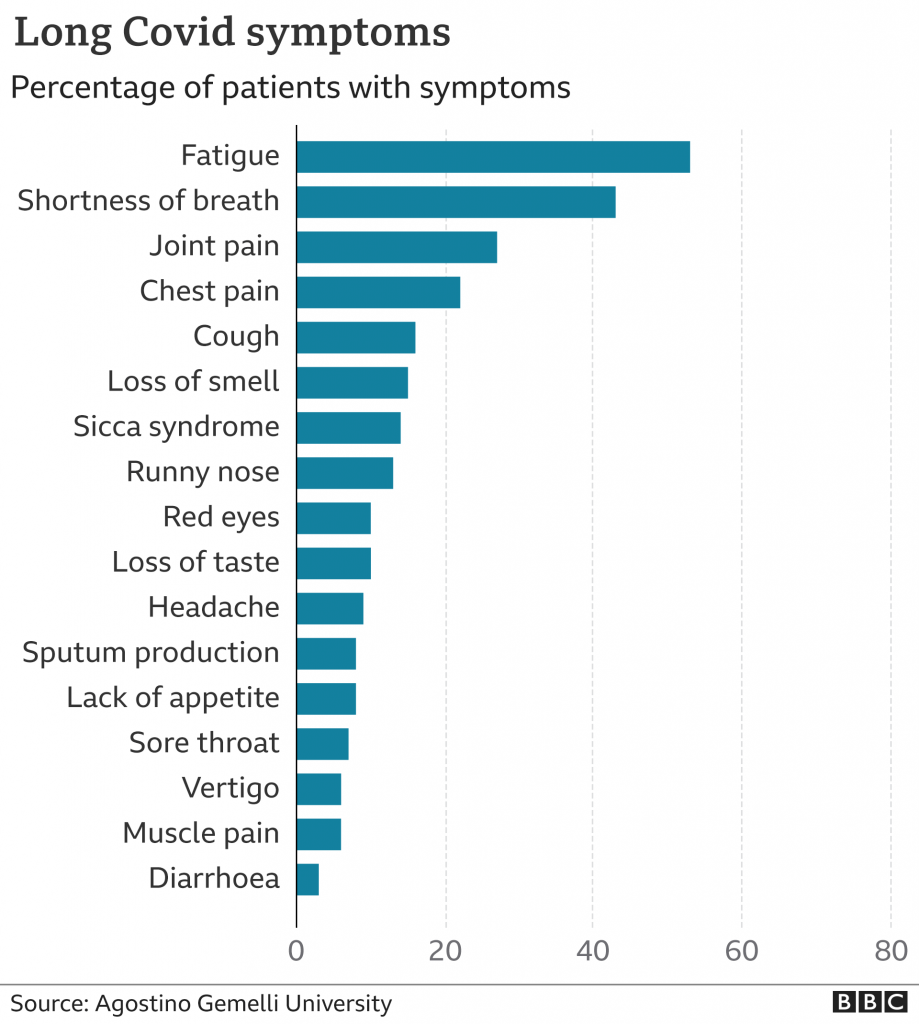
Long covid news of the day: The people who end up with long covid (as many as 1 in 5 covid cases do), are not the same as those vulnerable to severe, acute covid. The majority of long covid sufferers are under 45, and describe themselves as ‘youngish, fit, and healthy’. There are currently 3 or 4 main theories for what long-covid is, but the most promising is the hyper-immune system theory, where, after covid, the immune system would remain stuck in an over-reactive high gear. Or, as Gez Medinger the author of a recent study (1) on this explains: “…if you’ve already got an immune system that’s slightly trigger happy you’re going to find that trigger well and truly pressed by the covid juggernaught…” (This is a phenomenon that I am well aware of, it is already know in the world of ME/CFS and I will loop back to explain in another post, brain willing). This theory would suggest that people who have auto-immune, or immune dysfunction conditions, would be more likely to get long covid. Which Medinger went on to demonstrate, working with certain common conditions, amongst which was post-viral fatigue (PVF) which he found to be a staggering 6,000 times over represented in long-covid cases. i.e people who have had PVF and then contract covid, are extremely likely to get the long covid form.
PVF is ME/CFS. ME/CFS is a post-viral condition (most often after Epstein Barr virus). Some doctors will use the diagnostic term PVF, some will use CFS, some will use CFS/ME (this is current guidance in the UK), few will use ME/CFS, and very few will use ME – it depends on the doctor’s politics and how much they have read. Whilst in anycase a ME/CFS diagnosis requires 6 months of symptoms – before hand a more generalised PVF diagnosis will be given.
In the paper cited that derived this 6,000 times (2), PVF was selected out of a list of others – these included ME/CFS itself, Fibromyalgia, and aesthenia/debility. There is a lack of understanding of how these diagnostic terms operate in reality, there are no definitive tests for them, and though they are described here as distinct, they are all rather slippery. Here is a good example: because now my muscles are killing me due to long covid that my doctor still won’t recognise, he now believes I have Fibromyalgia rather then ME/CFS. The difference between these conditions is pretty much “what feels worse, muscle pain or fatigue?” that’s all. Though the 6,000 times over-representation is already extraordinary evidence to support the hyper-immune system theory and that people with ME/CFS are vulnerable to long covid along with those with other autoimmune or immune dysfunction, the 6,000 times is, in fact, a vast, vast under calculation too.
***********************************************************************************************
The thing about having ME/CFS, is that you have to spend a lot of time doing your own research. You get quite familiar with medical science. As an ME/CFS in-joke this is called a ‘PhD in ME’ – which is hilarious because nobody in the world of medical science has a certified PhD in ME. But, the point I was aiming to arrive to is that it shouldn’t be too-coincidental that I had ME/CFS and then got long covid. No – it should be predictable. It should be seen as a statistical likelihood. And I – and everyone else – should be believed.

I expect there are many people caught in this ME/CFS long covid blight. Many people thinking they are having the longest and worst flare of their lives, even though they have been doing everything right. There will be many people who have run out of sick leave by now, or used it up on the last flare and have nothing left to save them from having their jobs and livelihoods on the line (3). There will be people needing disability support who battled their whole life not to get to that point. I hope there are some people like me who have a generous sick leave from their PhD, though it can’t cope with 8+months. I am having to return to it not recovered, and it seems insurmountable. ME/CFS affects 600,000 people in the UK alone (4), millions of people worldwide, and probably millions more undiagnosed. It is also the least researched condition per people affected (5). So many of us will be stuck trying to reason with brick-wall-doctors over the phone answering back “no, you can’t seriously expect me to accept being critically disabled when I was nowhere near that stage before – it is long covid, for heavens sake”, and getting nowhere. And then going backwards when you try to talk medical science and their ego is tripped (I go for facts these days, not tears – it doesn’t work either).
I am half way through a second post, still putting off explaining what happened the last 8 months. What does it feel like? I’ve let the question hang in the air, because, as I mentioned, I’m still getting over my tendency to put off questions like that.
I know fatigue. I knew what to do when it arrived. What needs to happen to get through an ME/CFS flare, is the same as that needed to recover from long covid, roughly speaking. Long covid sufferers keep having relapses when they try to push through – this also might happen at the beginning when you think you have finished your 2 week recovery, and then don’t bounce back when you try. I didn’t try to bounce or push through right from the beginning. I took the pedal off the gas and made some space for rest. In the end this would prove not enough – it would turn out that I didn’t really know this new type of fatigue and illness at all.
The gas was off the pedal through March, April and the start of May. The lockdown was convenient for this – I must have been one of few people who benefitted. I had very painful legs – knee and ankle joints, and tingling, throbbing leg muscles – like hot lava inside not flesh and bone. My upper middle back hurt. I was surprised by the unrelenting desire to lie down. I did have fatigue but I could get through. I struggled to focus. My chest hurt, but it was a curious pain, like an internal aggravated itch. The chest pain didn’t follow exercise, not that I was exerting myself other than short walks. I was generally weak.
***********************************************************************************************
An ME/CFS factoid – The difference between tiredness and fatigue: Medically speaking, tiredness happens to everyone — it’s an expected feeling after certain activities or at the end of the day. Usually, you know why you’re tired, and a good night’s sleep solves the problem. Fatigue is a daily lack of energy; unusual or excessive whole-body tiredness not relieved by sleep. It can be acute (lasting a month or less) or chronic (lasting from 1 to 6 months or longer). Fatigue can prevent a person from functioning normally and affects a person’s quality of life (6).

Normally, the type of fatigue I receive with ME/CFS (it will be different for everyone) is like wading through mud. I can do most things though I’ll have to pick and chose, but it will be a pretty gruelling effort. It is a battle, and you learn to start the day with a battle cry (like a be-kilted Mel Gibson – not tears). In the years previous I have been lucky(?) with the ME/CFS – the fatigue had been present but manageable. Instead I had big difficulties with daily headaches, more acute light sensitivity, migraines, and gruelling gastrointestinal issues (this is a central nervous system thing, so communication breaks down for bodily things that should autonomous – in this case to my guts – i.e they just stop working.
In November to January prior I had been back and forth for ultrasounds and tests, and to make sure that it was only my guts sticking out and bruising the skin of my exceptionally swollen abdomen, and nothing more nefarious. Jumper season, thankfully. p.s if you do know me this is the reason I don’t eat gluten and dairy, I have to be gentle to my capricious guts. It is non-coeliac gluten sensitivity (NCGS) (7) – I.e no, I am not coeliac, and I don’t have crons disease either, but it is most defiantly real, and common with ME/CFS. There are a lot of real cases hidden inside of this profitable fad. I will also not eat much in company because my guts can suddenly seize and I won’t be able to bend my torso to leave the seat. I have an unreasonable fear of rye bread, potatoes, heavy sauces and a complicated relationship with food in general. I picked up smoking because it cures nausea (it used to be prescribed for morning sickness did you know?). It was really, really hard to quit. I also, if in a work-like setting, will eat the same thing everyday just because I know it will be ok. (I think people think I am autistic, and as I sit next to my friend with aspergers enjoying our same lunches and company together again, I am really ok with the assumption).
***********************************************************************************************
I digress, and so did my symptoms. Between May and June things got bad. In July I fell off the cliff and rocked up at A&E. Then I stayed 90% in bed through to September when I got up and got a puppy. Not because I was better, but because that was the limit of bed rest for my mental health.

I wasn’t resting as much in May – I was putting the gas back. I had a deadline and our jobs were being cut. We took a long walk to Sydenham forest, but I was spent before we got there (the fatigue had been getting worse), so we laid down on the Horniman grass short of our destination. When I stood up to go home I found that I couldn’t. My knees buckled, and my legs were not doing what they were told. In trying to walk I would veer off-course, and fall and catch myself every other step. I walked like walking really is, the repeating process of falling and catching yourself, and was supported in this by my partner B. The half hour walk home took 90 mins. I didn’t want to take the bus because of coronavirus. I didn’t know whether I had had it or not yet, but I was getting quite convinced the long covid working hypothesis was real. When we were most of the way home, a bunch of Lads in a VW golf, (all of the type left over from the 90s), yelled something inaudible though headphones which was visibly a dyke slur. We crossed the road, arms around shoulders and waists for support, and the car sped past pretending, very convincingly – shavingly even – to hit us. I was obviously struggling to walk. There was no chance I could run.
The breathing difficulties and chest pain got worse around then, and the chest and throat tightness arrived. In the next days and weeks and into June I was so overcome by fatigue, in episodes I couldn’t hold myself upright in a chair – not for lack or trying. I slipped off the chair mid-zoom meeting once, having the sense to turn my camera off first. I then lay gasping struggling with an elephant on my chest, so I turned my mic off too. It was at this point that holding a cup of tea felt like 10 kg. It was very strange. It felt like all the things in the world were suddenly extraordinarily heavy, rather then me being very weak. That, or somebody had gone around and stuck everything to the surfaces. I would go to pick something up and it wouldn’t come.

The chest pain and tightness became regular features. It stopped me from getting to sleep – had to prop myself high on pillows (and my painful legs still were still raised the other end). I would wake gasping in the middle of the night. At the end of June, after an episode of bad elephant-chest-squashing, I took a PCR covid test convinced that I currently had covid. It was negative. I called my doctor, who dismissed what I was feeling as a post-virus issue that would go away by itself. He said “it could have been a post-covid thing or not, it doesn’t matter, it will go”. I tried to live by his nonchalant vibes. I am angry that I did, as it would mean I would run out of time for the antibody tests to show anything, which got me in the position of treatment being even harder to get.
I rested, well, in June and I waited for the chest problems to fade. They did more or less, but I barely moved and kept my brain on permanent drivel mode. To be safe I waited 24 hours after symptoms, as that’s what the booklet said about when you should go out if your test was negative. We visited my parents (in the extremely vulnerable category). After 2 days I did an emergency handbrake turn and went home. The chest pain and breathing difficulty had come back with a vengeance, and I was terrified that I had brought covid to their door, even though B and I both had negative tests. We took another test when we got back, also negative. I called my doctor again, and received the same nonchalant response. I let my parents believe I had anxiety. For awhile I hoped it was anxiety too, I would take anything that had a solution even if it that meant mindfulness.
I tried to carry on, and manage the fatigue and breathing problems. In July the inability to walk home repeated. This time I couldn’t for the life of me walk in a straight line. I’m sure I looked completely pissed. I managed it half carried by B again. I tried to manage the fatigue, like I am used to. It wasn’t working. It wasn’t like I was sick in a normal way like, vomiting or having a fever. I didn’t want to be in bed all day. I could move sometimes, listen to podcasts, pretend like I was working, and exist around the flat, until suddenly debilitating fatigue would set in and if I didn’t sit I would fall, and if I didn’t lie down I would fold-over into a keyboard-face.
In late July, after resting in a way that I thought should be enough, I ventured a walk home alone, in the dark, for 30mins. Half way I again couldn’t walk in a straight line. I was falling into the road. My knees were not so often buckling this time, but my legs were well wayward. I was dizzy. My chest and throat were tight, my heart on a techno-rave. It was the worst I had felt it. This time I didn’t have B to help – she had gone to the beach on the train and still wasn’t back. She had cabin fever to resolve. I made the battle cry, and fell about in a forwardly way on a mission to get home. It was quite terrifying. I maybe should have called someone. Or got an uber. I could only think about needing to be home.
When I got home I landed on the couch and put on my oxygen and heart-rate finger monitor. I couldn’t read it because I was so dizzy (why are digital screens always red? so hard to keep the numbers still). My heart’s technobeat drummed off the scale. I pulled off all of my top-part clothes in the terror of not being able to breath. B found me slumped on the bathroom floor as I had needed to puke. I wanted to lie down for the nausea but it made the difficulty breathing worse. I’d fashioned a sick bucket out of the bin, by strewing the contents on the floor first. I was a mess. She put me to bed. It had subsided a bit. B knows about all of the ME/CFS stuff. We’ve been through some weird, potentially fatal symptoms together. We both know the drill. It was Sunday night. At the hospital all they do at the weekends and evenings is stabilise you and wait for the Doctor in the morning. Especially Sunday night. I was stable. It wasn’t a pneumonia. It wasn’t acute covid. It wasn’t a heart attack or a blood clot. And whatever it was the worst had relented. I went to A&E first thing the following morning after not much sleep. I brought a bag incase I’d be checked in.
To get into A&E with breathing problems during this covid crisis, I had to explain that I had 2 negative tests already. I showed them my emailed results. I was grilled about whether I had performed the test correctly (I did) and whether B also had the test and same result (she did). I’m glad this inquisition existed, only somebody who was actively lying could have coronavirus and get through. My ECG and lung X-ray were clear, my bloods were fine. I had my third negative covid test at the hospital too. The doctor believed what I was saying, I did mention that I thought it could have been long covid. The doctor took my family history. He was young. He looked a bit afraid of what I might have. I had a breast exam. I had to sit on the waiting room chairs and await the results and verdict, and listen to a woman at the seat along complain about how the whole world is against her that she would get an illness, how slow the nurses and doctors are, and taking a lunch break wasting her tax money etc etc. She went on like this to talking to herself and her patient tween daughter for 45-60mins, through a mask and through coughs and splutters. Then the doctor came, knelt down, held her hand, and gently told her she had coronavirus. And that she was fine enough and should take a taxi home, and not the bus she had used to get here. Poor taxi driver – on the frontline even more than we thought. The hospital didn’t shut down, there was no fuss, it was all made hush hush. I was sitting next to her for an hour, very ill people on stretchers were regularly passing. There very ill people everywhere – this was the heart and lung critical emergency sector of A&E. She then when on, whilst she was waiting for something or other, that it was dirty pigs that gave it to her. I wasn’t contact traced by the way, even though there are exceptional records that we were both there. I didn’t get it (again) then. I hope nobody else did either, but I don’t think that would be realistically true.
My doctor came with a piece of paper. I got gently asked to go into the cancer room – the quiet room – whatever you want to call it, that one room reserved for giving the shitty news, the one with the sofa, bad art and magnolia walls. He was nice, the doctor, he cared. He told me, given my sporadic breathing difficulties and heart racing, plus this big lump on my neck that I had long since ignored, that it was his and the consultants recommendation that I had Hodgkins Lymphoma. This was my referral letter, I should expect a call and an appointment within 2 weeks. My grandma had it so I know what it is and how horrific it is. I told the nice doctor not to fret, that there was no need to be so worried, that I was used to hearing terrible possible diagnosees, that I handle that wait to hear ok by now, and that it really was quite likely to be my old friend ME, so give yourself a break, it’s ok. I also asked to have 10 mins to lie on the couch, because the fatigue was really bad and I had to have a moments rest so I could get home.
So far, in my brain-foggy way – which is to have a lack of ability to summarise, and the mislaying of executive function – I have just arrived to mid July. There is the rest of July, August, September, October and November to go.
1 – Gez, Medinger. Who Gets Long Covid, and Why?, Huge Findings From New Study, 2020. https://www.youtube.com/watch?v=hnPvw20iH80&feature=youtu.be&t=2s
2 – Collin, Simon M, Inger J Bakken, Irwin Nazareth, Esther Crawley, and Peter D White. Trends in the Incidence of Chronic Fatigue Syndrome and Fibromyalgia in the UK, 2001–2013: A Clinical Practice Research Datalink Study. Journal of the Royal Society of Medicine 110, no. 6 (June 2017): 231–44. https://doi.org/10.1177/0141076817702530
3 – The Guardian. I Had Long Covid – but Not Everyone Gets Time to Recover, Amelia Horgan, 3 November 2020. http://www.theguardian.com/commentisfree/2020/nov/03/long-covid-time-recover
4 – Rutherford, Gina, Philip Manning, and Julia L. Newton. Understanding Muscle Dysfunction in Chronic Fatigue Syndrome. Journal of Aging Research 2016 (2016). https://doi.org/10.1155/2016/2497348
5 – Radford, G, and S Chowdhury. ME/CFS Research Funding. An Overview of Activity by Major Institutional Funders Included on the Dimensions Data Base. Action for M.E, 2016. https://www.meassociation.org.uk/wp-content/uploads/mecfs-research-funding-report-2016.pdf
6 – WebMD. What Is the Difference between Tiredness and Fatigue? Accessed 11 November 2020. https://www.webmd.com/multiple-sclerosis/qa/what-is-the-difference-between-tiredness-and-fatigue
7 – Biesiekierski, Jessica R, and Julie Iven. Non-Coeliac Gluten Sensitivity: Piecing the Puzzle Together. United European Gastroenterology Journal 3, no. 2 (April 2015): 160–65. https://doi.org/10.1177/2050640615578388